Posterior Vitreous Detachment (PVD)
What is PVD (posterior vitreous detachment)
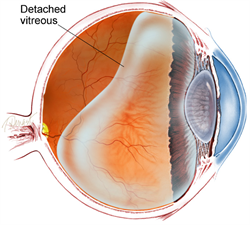
When the gel that covers the eyeball separates from the retina, it results in posterior vitreous detachment (PVD). The thin layer of nerve tissue that lines the back of the eyeball called the retina. It’s in charge of recognizing light and converting it into pictures.
Your eyesight may become more frequently dotted with grey or black shadows or flecks after PVD. Additionally, it could cause bright flashes to appear, usually to the side of your eyesight.
Causes
Due to ageing and normal wear and tear, the vitreous gel that fills the eye condenses (shrines) with time. The gel eventually runs out of space in the eye’s vitreous cavity, which positioned at the very back of the eye cavity and stays the same size throughout maturity. As a result, the gel separates from the retina.
The space between the condensed vitreous gel and the retina filled with clear vitreous fluid.
The symptoms of a PVD are often modest if it develops slowly, consistently, and uniformly. However, the PVD can rupture the retina or a retinal blood artery if the forces of separation are severe or concentrated in one area of the retina, or if there is an abnormal adhesion (sticking together) between the vitreous gel and the retina (such as lattice degeneration). When PVD made more severe by a retinal tear or vitreous haemorrhage, flashes and floaters are often more noticeable. These abnormalities can develop into more serious problems like epiretinal membrane or retinal detachment, which can impair vision permanently.
However, nearly 85% of individuals with PVD never encounter difficulties, and the flashes and floaters often go away in 3 months.
RISK ELEMENTS
In adults under the age of 40, posterior vitreous detachment is uncommon, but as people get older, it becomes more frequent.
Myopia (nearsightedness), trauma, and recent eye surgery, such as a cataract procedure, are additional risk factors for PVD. Within a year, patients who have PVD in one eye are frequently diagnosed with PVD in the second eye as well. For any help, Contact our best eye doctor in west delhi at bharti eye foundation
How to diagnose PVD
Despite the fact that PVD is frequent, it’s crucial to see our best eye doctor if you start experiencing new floaters or flashes. A retinal detachment or PVD may be the cause of these. To diagnose your problem, your doctor might need to run a diagnostic test.PVD, a retinal detachment. Our best ophthalmologist or optometrist will insert special drops into your eyes during the examination. Our best eye doctor can view the back of your eyes thanks to these drops since they make your pupils bigger. The entire retina, the macula, and your optic nerve can then examined through our best eye specialist.
Other tests
Additional tests may occasionally required to diagnose PVD.
For instance, it could be challenging for our eye doctor to spot a separation if your vitreous gel is exceptionally transparent. In such a case, the condition can identified using an ocular ultrasonography or an optical coherence tomography.
Ocular ultrasonography employs high-frequency sound waves to provide a picture of your eye, whereas optical coherence tomography uses light to produce a three-dimensional image of your eye.
Treatment
The floaters or flashes typically go away in three months, but three months following your diagnosis, you should have another dilated eye exam to make sure your retina hasn’t suffered any new harm.
After a few months, if you still have significant floaters, your doctor may suggest using a laser to lessen the floater or having surgery to remove the vitreous gel and remove the floaters.
A retinal tear can fixed using laser surgery or cryopexy, which freezes the tear.
What activities am I still able to undertake despite having PVD?
The majority of patients with pvds unrestricted in their ability to engage in daily activities. High impact exercise advised to avoided for the first six weeks after the onset of a PVD, according to some ophthalmologists. This is due to the possibility that your vitreous has not fully separated from your retina, and you may be more susceptible to developing a retinal detachment at this time.
Although there is no proof that any of the following behaviours will unquestionably lead to PVD issues, some persons may advised to avoid them or opt to do so:
Exercises requiring a lot of energy or strong impact, such jogging or aerobicsdoing contact sports, like rugby, boxing, or martial arts.
Inverted poses used in exercises like yoga and pilates.
Always seek the opinion of your ophthalmologist regarding which activities and for how long you should refrain from engaging in them. The advice you receive may depend on whether your retina thought to be particularly at danger.
If you do engage in any of these activities, you might become much more aware of your floaters. This is due to the fact that these activities need you to move about, which can cause your floaters to move around inside your eye more. As a result, you might want to put a stop to such activities until your brain adjusts and learns to disregard your floaters.
You can continue doing things like walking, light exercise, reading, watching TV, cooking, and using your computer on a daily basis. There is no evidence to support the idea that taking an aircraft can aggravate or worsen your PVD. Additionally, wearing makeup or contact lenses has no impact on your PVD.
Clinical presentation
Sudden onset “floaters” in one’s visual field are most frequently caused by PVD, which is more accurately referred to as “vitreous condensations” in this context. It may also result in photopsia, which made worse by eye movements.
Radiographic characteristics
Ultrasound
The following traits can seen in the isolated posterior vitreous detachment’s sonographic appearance:
- Membrane that is linear and echogenic in the back compartment
- There may be thickening if there is bleeding or inflammation.
- May show tethering close to the ora serrata
- Vitreous base refers to the point of attachment
- Using oculokinetic ultrasonography, without restriction
- The membrane will cross where the optic nerve sheath and posterior wall of the globe meet, unlike retinal detachment.
- PVD should have demonstrate “after movements” in the acute stages that are more evident than what would anticipated from retinal/choroidal detachments
- Mobility may diminish over time, making it challenging to distinguish from other vitreous diseases.
- May linked to further pathologic symptoms, such as;
- Retinal twitching
- Vitreous bleeding
Also Read:





